NCD Policy Toolkit
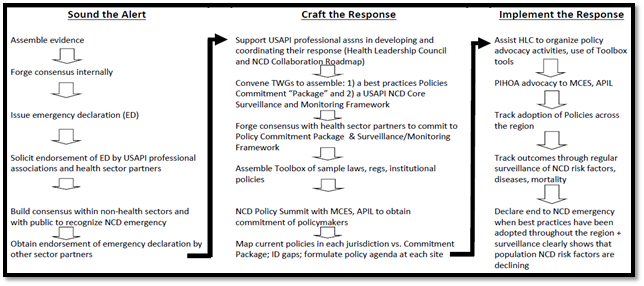
In May 2010, the health officials of the US-affiliated Pacific Islands (USAPIs) joined together in a landmark decision to Declare a Regional State of NCD Emergency: Pacific Island Health Officers Association (PIHOA) Resolution #48-01. It was a critical decision that pulled together the USAPIs in responding to the NCD crisis in ways the region had never experienced, and triggered high-level USAPI responses and commitments across executive and legislative branches of government, and traditional leadership. Following the declaration, an ‘incident command’ response framework (USAPI NCD Strategic Roadmap) was developed to inform the regional response over three key phases:
1. Sounding the Alert: raising awareness and advocacy amongst key decision-makers in the USAPIs and across the wider Pacific;
2. Crafting the Response: developing NCD-related tools and resources and establishing effective partnerships, and
3. Implementing the Response: adoption of an agreed package of NCD policies and legislation, convening a USAPI NCD law and policy summit, collection and analysis of NCD data and information to track NCD progress and risk factors.
- Home
- Introduction
- Declarations
- Policies 101
- Engagement
- Tobacco
- Alcohol
- Nutrition
- Physical Activity
- Health in All Policies
An Introduction to the NCD Policy Toolkit

Dear Pacific Colleagues,
Iakwe kom, kaselehlie maing, len wo, mogethin, hafa adai, ran annim, talofa and alii!
I have the ultimate pleasure to present to you the USAPI NCD Policy Toolkit. It has been a long road to travel in achieving this significant milestone for the Pacific region since an NCD emergency was declared in May 2010. This toolkit has been made possible through the hard work, dedication, passion and commitment of many individuals and organizations over the last couple of years. Most especially, I wish to thank the University of Hawaii John A. Burns School of Medicine, Department of Family Medicine and Community Health team, for their tireless work in researching, developing, refining, editing and putting together in a cohesive and coherent manner, this very important tool and resource which will guide and inform critical work to address NCD risk factors through the adoption of appropriate policies and legislation in the USAPIs. Below is a summary background of when, where and how the USAPI NCD Response began, and the critical next steps in our continued response to reducing the impact of NCDs on our island communities and families.
We hope you will use this toolkit to its maximum potential!
Respectfully,
Emi Chutaro
Executive Director
PIHOA Regional NCD Response Timeline (2010-2019)
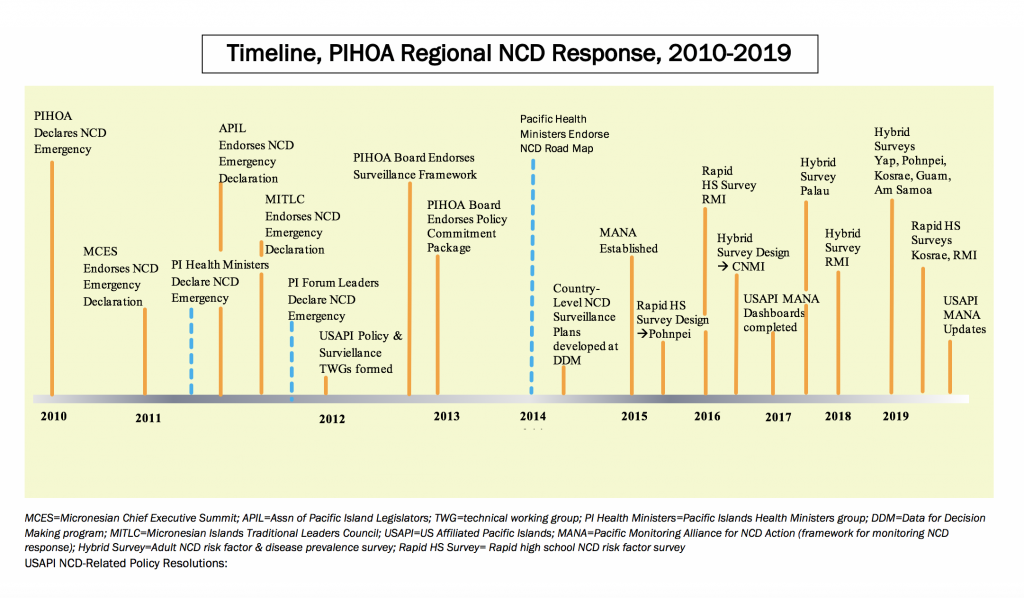
In June 2012, PIHOA assisted to establish the Health Leadership Council (HLC) as a regional coordination body to bring together a network of existing USAPI professional associations and strengthen partnerships and synergies to address NCDs. The HLC Terms of Reference was developed and endorsed by the USAPI health officials in June 2013, including the USAPI NCD Roadmap which informs and guides NCD work across the HLC members. This was to capitalize on existing NCD interventions and content-area expertise available through the regional professional associations, and to strengthen and enhance collaborative responses to NCDs in support of the USAP NCD emergency response as mandated by the USAPI health officials.
In early 2012, PIHOA also convened two regional technical working groups (TWGs) to discuss and develop a regional NCD surveillance framework and regional NCD policies. In 2013, the USAPI health leadership reviewed and endorsed the USAPI NCD Core Monitoring and Surveillance Framework (and Data Set), as well as the USAPI NCD Commitment Package addressing common NCD risk factors: alcohol and tobacco use, lack of physical activity and poor nutrition.
With wide endorsement and support of the USAPI NCD Commitment Package and a call to convene a USAPI NCD Law and Policy Summit, a USAPI NCD Toolkit needed to be developed to guide and inform NCD policy development appropriate to the USPAI context. In early 2014, PIHOA contracted the University of Hawaii John A. Burns School of Medicine, Department of Family Medicine and Community Health to develop an online NCD toolkit embedded within the PIHOA website. Drafts of the online toolkit were vetted and peer reviewed on several occasions across different regional meetings and forums throughout 2014. CD-ROMs of the toolkit were made and distributed to the USAPIs in 2015.
Next steps will include continued work with the USAPIs to utilize this important resource in advocating, promoting, developing, adopting, implementing and monitoring NCD policies and legislation. By having comprehensive, supportive and enabling NCD policies and legislation in place to address key risk factors, significant strides will be made in reducing the negative impact of NCDs on our islands and communities.
USAPI NCD Strategic Roadmap
USAPI NCD Surveillance Framework
Acknowledgements
This USAPI NCD Policy toolkit was made possible primarily with funding from PIHOA’s United States Center for Disease Control (CDC) National Public Health Improvement Initiative (NPHII) Grant, as well as additional funding support from PIHOA’s CDC Association of State and Territorial Health Officials (ASTHO) project funds. Technical support for the development and refinement of the toolkit was made possible by the generous support and expertise of the University of Hawaii John A. Burns School of Medicine (JABSOM), Department of Family Medicine and Community Health team and PIHOA Secretariat staff, the Health Leadership Council, Secretariat of the Pacific Community, CDC Chronic Disease, and the USAPI national and state NCD programs. In particular, PIHOA would like to thank:
UH JABSOM Team
- Dr. Lee Buenconsejo-Lum
- Dr. Neal Palafox
- Mavis Nitta
- Dioreme
- Janos Baksa
PIHOA Secretariat Team
- Michael Epp
- Dr. Mark Durand
- Dr. Gregory Dever
- Jason Aubuchon
- Emi Chutaro
- Billie Hiraishi
CDC Team
- Roberta Erlwein
- Suzanne White
- Loren Cadena
Health Leadership Council
- Va’a Tofaeono
- Patrick Luces
- George Cruz
NCD Declarations and Executive Orders
Key Pacific NCD Policy Declarations
Key Pacific NCD Policy Executive Orders
Health Policies 101
Policy 101 section aims to provide overarching policy-making information that could be taken by each jurisdiction and customized, depending on the needs, resources and customary practices of the jurisdiction. The goal of this section is to provide a concrete and valuable resource for individuals, government agencies and community-based organizations in the United States Affiliated Pacific Islands (USAPI) in activities related to health policy-making in the local and national level. Containing six subparts, each addressing components related to health policy planning and implementation processes, this section aims to be a one-stop resource for all USAPI policy-related needs. Policy 101 is broken down into 6 subparts:
(1) Policy 101
(2) Things to Consider: Intended and Unintended Consequences of Policies
Focusing on the general to specific steps in the policy-making process—from departmental assessments, garnering support from key stakeholders, drafting a bill, and ultimately, to passing and implementation
(3) Capacity Building
(4) Appendices
(5) Supplemental Materials
(5) Additional Resources
Policy Engagement and Collaboration
Engagement and Collaboration section aims to provide overarching policy-making information that could be taken by each jurisdiction and customized, depending on the needs, resources and customary practices of the jurisdiction. Engagement and Collaboration section focuses on tools and techniques in effective community engagement between wide groups of people to multisectoral partnerships beyond the health sector. This section encompasses practical templates of community engagement planning as well as best-practices from other communities that could be valuable and adaptable to the USAPI. It also emphasizes sustaining stakeholders’ support and political momentum through collaboration. It incorporates cultural considerations in collaboration activities, as well as guiding principles for public policy and community action. Engagement and Collaboration is broken down into 3 subparts:
(1) Community Engagement and Collaboration
Includes guides that may be useful when working with traditional and cultural leaders, and tools and guides for multisectoral partnerships as well as stories from the Pacific related to collaborative works.
(2) Appendices
(3) Supplemental Materials
What you should know about tobacco?
Tobacco is the only product sold in the USAPI that when used as instructed kills people. It is the only legal way to kill someone. It is a major risk factor for all major NCDs, including cardiovascular disease, diabetes, cancer and chronic respiratory disease.
Why is it important?
- Tobacco kills up to half of its users.
- Nearly 80% of the world’s one billion smokers live in low- and middle-income countries.
- The US-Affiliated Pacific Islands have very high rates of tobacco use:
| Tobacco Use in the USAPI | Youth | Adults |
|---|---|---|
| Marshall Islands | 25.9%1 (any tobacco use) | 19.8%7 (current daily smokers) |
| Palau | 50.3%2 (any tobacco use) | n/a |
| FSM | 37.0%3 (other tobacco use) | 31.6%8 (current smokers) |
| Guam | 23.1%4 (current smokers) | 27.4%9 (current smokers) |
| American Samoa | 24.2%5 (current smokers) | 29.9%10 (current smokers) |
| CNMI | 23.9%6 (current smokers) | 21.8%11 (current smokers) |
- It is estimated that two people die each minute from tobacco-related disease in the Western Pacific Region.
- Secondhand smoke causes premature birth and miscarriages in pregnant women.
- Secondhand smoke has immediate negative effects on the cardiovascular system, which can cause lung cancer and heart disease.
What you should know about alcohol?
The misuse and abuse of alcoholic beverages is a public health threat. It can lead to injuries, liver cirrhosis, cancers, cardiovascular diseases, and premature deaths. Socially, alcohol misuse and abuse can lead to poverty, family and partner violence, and poor social acceptance. Effective alcohol policy will help to reduce the prevalence of alcohol-related injuries, cardiovascular disease, cancers of the mouth and throat, esophagus, stomach, and liver, premature deaths, and disabilities. It will also improve the quality of life for individuals and communities, and potentially improve the socio-economic status of those otherwise affected by excessive alcohol use.
Why is this important?
- Alcohol is the leading risk factor for disease in the Western Pacific.
- In some Pacific Islands, the coconut toddy, or also known as tuba, can be distilled into an alcoholic drink. It is a source of cheap unregulated alcohol and has a high content of alcohol.
- Alcohol use causes harm to the individual and the people around them. Alcohol use is linked to violence, crime, sexual abuse, road traffic accidents, and loss of work, putting others at risk or danger.
- Alcohol drinking by mothers is harmful to the health of the developing fetus.
- Almost 10% of all deaths for young adults ages 19-29 are due to alcohol-related causes.
What you should know about nutrition?
Traditional foods typically have a high nutrient content and provide energy needed for active lifestyles. Unfortunately, the Western influence has brought the islands canned meat, soda, white rice, and junk food, all of which are high in calories and low in nutrients. Pacific communities that once were self-sustaining are now dependent upon unhealthy imports for food. Eating habits are established in childhood, and the availability of cheap processed foods (versus local foods) determines what youth eat. Unhealthy food habits lead to obesity, disease and death. With effective food policies we will see a decrease in obesity among children – within 1-2 years – and decrease in disease and death in adulthood.
Currently, much of the food that is easily available, accessible, and affordable in the USAPI, is unhealthy. There are few options for people to choose healthy foods and beverages with the competing demands of work, culture, religion, and social obligations. High rates of non-communicable diseases in the USAPI region suggest that food consumption patterns need to change. To facilitate this movement, policies can be implemented.
Why is it important?
- In the Western Pacific Region obesity prevalence is highest in the Pacific countries, where some of the highest rates of overweight and diabetes are found.
| Obesity Rates (BMI > 30 kg/m2)* | Diabetes Rates* | |
|---|---|---|
| American Samoa | 75% | 47% |
| Federated States of Micronesia | 43% | 32% |
| Republic of the Marshall Islands | 45% | 28% |
| U.S. Aggregate | 33% | 8% |
- Poor nutrition can contribute to stress, tiredness and reduced capacity to work.
- Poor dietary choices can lead to conditions related to malnutrition, which include a weakened immune system and long-term chronic diseases, such as high blood pressure, high cholesterol, heart disease, diabetes, cancer and gout.
What you should know about physical activity?
In the past, Pacific Islander communities were active farming, fishing, building, dancing, walking, and swimming. Today, communities move less and consume more calories than they burn. Cars reduce the need to walk. Many people are employed in jobs where they sit all day long. The result is an inactive population with high rates of obesity and non-communicable diseases, such as cancer, diabetes and heart disease. Establishing policies that support active lifestyles is critical for healthy communities.
Why is it important?
- Physical inactivity is considered one of the main risk factors contributing to obesity and related diseases in both developed and undeveloped countries.
- Globally, approximately 3.2 million deaths each year are attributable to insufficient physical activity.
- Since 1980, obesity prevalence among children and adolescents has almost tripled in the U.S.
- Exercising just 30 minutes of day can reduce your risk of heart disease, diabetes, and cancer. For older adults, physical activity can improve mental function.
What Should you Know About Health in All Policies?
Health in All Policies (HiAP) is an approach to policy development and implementation that considers the social and environmental implications of its decisions. It recognizes that other factors beyond healthcare can have a significant impact on health and the community’s well being. HiAP encourages other sectors to get involved and inform decisions in policies. Through partnership, connections can be thoroughly examined allowing a broader perspective in the process of policy making and a more effective approach to improving the health outcomes and health equity of communities.
HiAP was first coined in the early 1990s, however, it was more thoroughly defined in 2006 during the Finnish presidency of the EU. It’s tougher approach through strengthening existing legislation and implementing policies through cooperation across sectors, influenced others to adopt a HiAP approach. HiAP strategies can now be seen in countries worldwide, such as Australia, Iran, Cuba, Norway and Thailand. Its implementation and incorporation across varying degrees of political organization and socioeconomic status illustrate its feasibility regardless of a country’s development.
Plans for environmentally sustainable communities in California, tighter tobacco regulations in Brazil and tougher child protection policies in Chile, are just a few examples of the way HiAP models are making significant achievements in health and challenging their country’s biggest health problems. Its feasibility lies in its collaborative and cohesive approach and its promotion in “doing the best possible within the context of political will and resources” (WHO).
NCD Policy Toolkit: Intervention #13–Encourage Built Environments
Develop a Built Environment to Promote Physical Activity
The environment in most island communities no longer promote physical activity. Roads and unleashed dogs discourage walking and make exercising outdoors dangerous. Unfortunately, most schools and workplaces do little to encourage or value movement. The built environment (i.e. parks, walking trails) is one of many variables that can increase physical activity.
Outreach Materials
For more information and how to get involved, here are links to materials for different target audiences. The fact sheets and presentations includes key facts and resources, along with sample policies, that support the intervention. These documents should be adapted for your community with local data and resources.
Here are additional resources to help you get started:
Framework Convention on Tobacco Control